This article discusses a mental health condition and mentions suicide and suicidal ideation.
Changes in mood are normal and experienced by everyone, according to the National Institute on Mental Health (NIMH). However, when those temperament changes are extreme and affect how you think and act, it could be classified as bipolar disorder (via Cleveland Clinic). Formerly referred to as manic depression, this mood disorder interferes with the everyday life of close to six million Americans (via NIMH).
Bipolar disorder affects men and women almost equally, and symptoms generally begin around age 25 for both sexes. However, women with this illness are more likely to be misdiagnosed and treated for depression instead of bipolar disorder. Men with bipolar disorder tend to be misdiagnosed and treated as schizophrenic, according to the Depression and Bipolar Support Alliance (DBSA).
The mood changes associated with bipolar disorder often come in waves that last hours, days, or weeks. However, even though they come and go, the condition is considered chronic, and treatment is a lifetime commitment (via NIMH).
Causes of bipolar disorder
Medical professionals point to two factors that make a person more prone to developing bipolar disorder: genetic makeup and a chemical imbalance in the brain (via UNC Center for Excellence in Community Mental Health). Close family members with bipolar disorder make it more likely for you to be diagnosed with the mental illness.
Doctors point to the brain when determining the origin of mental illnesses, including bipolar disorder. Specifically, medical professionals look at the three chemicals called neurotransmitters that are required to be balanced for your brain to function properly. They are noradrenaline, serotonin, and dopamine. Bipolar episodes occur when these get out of whack (via NHS).
Genetics and chemical imbalances make you more prone to a bipolar diagnosis. However, these two factors don’t always work on their own to produce a bipolar episode. Instead, stressors need to be introduced for symptoms to occur. Common aggravators of this condition include life events like births, deaths, new jobs, and the onset of other illnesses and depression (via UNC).
Diagnosing bipolar disorder
Bipolar disorder is diagnosed in two stages. The first phase is to have your mood episodes diagnosed to determine if they fall into the categories of mania, hypomania, or depression. From there, your doctor will then take steps to determine if you have bipolar disorder (via American Psychological Association).
Medical professionals use a multistep approach to properly diagnose patients with bipolar disorder (via Cognitive and Behavioral Practice). The evaluation begins with reviewing the medical histories of the patient and their immediate family. Chances of being diagnosed with bipolar become exponentially greater the closer a previously diagnosed relative is to you (via APA). The doctor will also ask several specific questions and request that you complete screening tools. These will assist your medical provider in eliminating other issues, including additional illnesses, drug addiction, and life stressors like a new job or a recent move. To ensure a proper diagnosis, doctors use a probability-based approach to identify bipolar disorder. They consider several factors, including risk factors, scale scores, and diagnostic probability of treatment need (via Cognitive and Behavioral Practice).
Manic episodes
Master1305/Shutterstock
Doctors cannot diagnose bipolar disorder unless you have gone through at least one incident of either mania or hypomania, according to the National Association on Mental Illness (NAMI). Manic episodes, or mania, are described as periods in which you feel better than ever. It’s almost as if you are high without taking any drugs. Your energy level is through the roof, and you are enthusiastic about everything (via NAMI). These periods of mania often begin with some telltale signs that become more recognizable after diagnosis. These include wearing more flamboyant clothing, faster driving, and being more agitated and defensive (via Health).
Manic episodes vary from person to person, but often include periods where you have lots of energy yet require little sleep. You talk faster and louder, and you are more easily distracted. Often, those going through a manic episode participate in dangerous activities. You may spend money you don’t have, try drugs, or have unprotected sex. Episodes of hypomania are similar, but generally hypomania is considered less severe in that it won’t as clearly cause issues in one’s day-to-day life. If you or someone you know is experiencing extreme symptoms of mania, including suicidal ideation, seek immediate help (via Verywell Mind).
Depressive episodes

Shift Drive/Shutterstock
Everyone feels sad occasionally. However, those with bipolar disorder may experience a major depressive episode in addition to the mania required for diagnosis (via Verywell Mind). A major depressive episode lasts more than two weeks. Episodic symptoms involve feeling dejected and apathetic. To be properly diagnosed, you also must encounter a change in one of several life factors. These consist of an increase or decrease in eating, sleeping, and overall enthusiasm for life. A major depressive episode may also include issues with making decisions, feeling suicidal, and feeling worthless. Those experiencing a major depressive episode may appear angry or agitated instead of sad or depressed. Additionally, the mood changes you experience must significantly interfere with your everyday life to be considered a major depressive episode (via Psycom).
Those with bipolar disorder who experience depressive episodes report that they last up to three times as long as both manic episodes and hypomania. Doctors rule out depressive episodes in patients with other medical conditions or who take prescribed and illicit drugs (via Verywell Mind).
Mixed episodes

Sotnikov Misha/Shutterstock
In addition to the manic episodes required for diagnosis and the depressive episodes, around 40% of those with bipolar disorder report experiencing mixed episodes (via CNS Drugs). However, according to Dr. Harvinder Singh, mixed episodes are underdiagnosed compared to manic and depressive issues (via Psychiatric News). Dr. Singh also reveals that those with mixed episodes usually present symptoms at a younger age and take longer to be properly medicated. These factors make patients with mixed episodes more likely to experience psychotic episodes, be hospitalized at a greater rate, and commit suicide in more significant numbers.
A mixed episode is a period wherein you experience symptoms of both mania and depression (via Healthline). This means that you have a manic episode with symptoms of depression or a depressive episode with feelings of mania (via PsychCentral). In other words, during a manic episode, you also experience exhaustion and move slower, feel disinterest in your favorite activities, or have feelings of worthless or even experience suicidal ideation. You are both ecstatic and sad or angry. You may be hyperfocused but fail to get much done because you are impulsive, reckless, and distracted. A depressive episode with manic features includes feelings of euphoria, talkativeness, and less of a need for sleep (via PsychCentral). Your emotions might be erratic and, if accompanied by psychosis, get worse.
Bipolar I

Doucefleur/Shutterstock
There are several types of bipolar disorder. Each variation has its own set of diagnostic criteria. Bipolar I requires patients to suffer from a manic episode that lasts at least a week, or that the patient requires hospitalization due to the seriousness of their symptoms (via NIMH). The manic episode often includes feelings of anger or euphoria with excess energy. Those with bipolar I may experience periods of normalcy, depression, or psychosis. However, depression and delusion are not required for diagnosis (via APA). Many patients with bipolar I are first diagnosed with major depressive disorder. Unfortunately, reaching a proper diagnosis takes up to 10 years (via Johns Hopkins Medicine). Several common conditions often accompany bipolar I. Therefore, physicians treating patients with bipolar I should watch for substance abuse, anxiety, and panic disorders.
Though both women and men with bipolar one tend to get equally diagnosed around age 20, women are prone to mania. Women with bipolar I can have more than four manic episodes a year. Additionally, pregnancy offers women another stumbling block. It’s best to speak with your doctors to determine if you should continue your medication while pregnant. You risk a relapse if you stop taking your prescriptions. However, those drugs could be harmful to the unborn child.
Bipolar II
Miriam Doerr Martin Frommherz/Shutterstock
Many people mistakenly believe that bipolar II is not as severe as bipolar I. This is because the mania associated with bipolar II is not as extreme as that experienced during bipolar I. However, the depressive episodes endured as part of bipolar II tend to be more serious (via PsychCentral). The depressive episodes associated with bipolar II often include symptoms of a lack of energy and motivation. You may also feel hopeless and numb, or turn to unhealthy food for comfort (via Healthline). You might also sleep more. These symptoms lead to the misdiagnosis and treatment of over 10% of patients who get treated for major depressive disorder (via Annals of General Psychiatry).
For a proper diagnosis of bipolar II, a patient must also experience a period of hypomania. Many who experience hypomania can function normally. However, those around them notice subtle differences, and the symptoms can be dangerous. They include hyperactivity, irritability, loudness, fast talking, and risk taking (via Healthline).
Though anti-depressants are commonly prescribed for bipolar II, they can trigger hypomania in some. Therefore, doctors should monitor you closely, and you should keep a log of your emotions (via PsychCentral).
Cyclothymic disorder
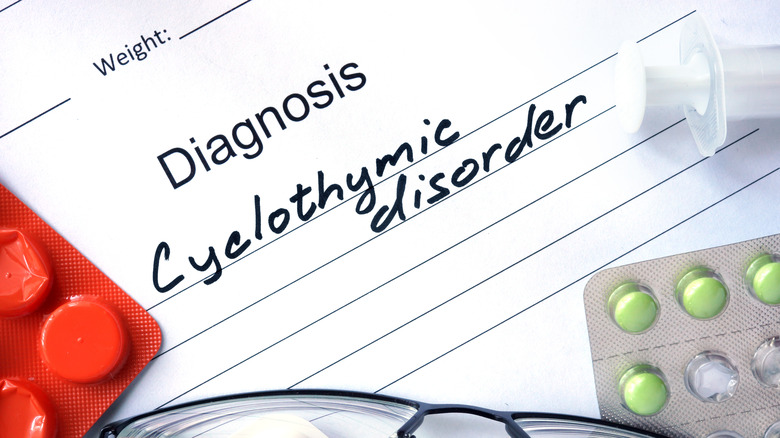
Vitalii Vodolazskyi/Shutterstock
Doctors consider cyclothymic disorder the mild form of bipolar disorder. Those with this diagnosis do not go more than two months without experiencing either hypomania or depression (via MedlinePlus). Though those with cyclothymic disorder may feel tired or wired, the lows and highs aren’t intense enough to cause interruption to everyday life, but they do occur often. Patients with cyclothymic disorder experience normal moods in between mood swings (via NHS).
To be diagnosed with cyclothymic disorder, children must have symptoms for over a year, and adult symptoms must be present for at least two years (via Healthline). Cyclothymic disorder is rare. It occurs in less than one percent of men and women, and typically first presents during adolescence or young adulthood (via Psychology Today). Up to 50% of those diagnosed with cyclothymic disorder are diagnosed with either bipolar I or bipolar II. Substance abuse and anxiety disorder are also commonly diagnosed in those with cyclothymic disorder.
Comorbidities with bipolar disorder

Billion Photos/Shutterstock
There are a number of other mental health conditions that are often also diagnosed in people with bipolar disorder. For instance, over half of those diagnosed with bipolar disorder develop an anxiety disorder (via World Journal of Psychiatry). Additionally, panic disorder affects 20% of bipolar patients (via Psycom). Panic attacks are most prevalent in those who experience depressive and mixed episodes and cause feelings of terror to the point that you feel dizzy with strong heart palpitations.
Post-traumatic stress disorder (PTSD) results from being a part of a disturbing situation, and common symptoms include flashbacks, insomnia, and nightmares. In those with both bipolar disorder and PTSD, the conditions provoke each other, with bipolar episodes causing their own trauma that then exacerbates the symptoms of PTSD. For those with bipolar disorder and obsessive-compulsive disorder (OCD), the symptoms generally appear during depressive episodes. However, repeatedly doing an activity tends to go away during manic/hypomanic episodes.
Three common anxiety co-diagnosis for those with bipolar disorder include generalized anxiety disorder (GAD), where you worry abnormally over ordinary things for at least six months, social anxiety disorder (SAD), where human interaction causes nausea and self-consciousness, and phobias (via Psychiatric Times).
Bipolar disorder and borderline personality disorder (BPD)

Yeexin Richelle/Shutterstock
Medical professionals first included borderline personality disorder (BPD) as a medical diagnosis in 1980. However, many argue it should be considered a type of bipolar disorder due to its similarity (via Verywell Mind). Common behaviors that both disorders include are impulsiveness, intense emotions, and suicidal thinking (via NAMI). Like those with bipolar disorder, patients with BPD experience mood swings. The difference is that those with BPD rarely experience periods of normalcy. Instead, they are in a constant state of mood changes (via Health Matters).
An overlap in diagnosis occurs 10% of the time for those with bipolar I and 20% of the time for those with bipolar II (via Dialogues in Clinical Neuroscience). In addition, those with dual diagnoses of both disorders are often told they have bipolar first because medical professionals need additional time to identify BPD (via Healthline).
Those who experience the psychosis associated with bipolar I are easier to diagnose, as those characteristics are not associated with BPD (via NAMI). Additionally, three-quarters of those with BPD engage in self-harm (via National Education Alliance for Borderline Personality Disorder).
Psychotherapy treatment

Prostock-studio/Shutterstock
Psychotherapy treatment incorporates methods that help patients relieve stress and function better in society (via ScienceDirect). Patients get information that helps them better understand their illness and how to deal with its associated symptoms and triggers. Incorporating psychotherapy into the care given to those with bipolar disorder decreases relapse rates nearly in half over medication alone (via The Medical Journal of Australia).
One common type of psychotherapy is cognitive behavioral therapy (CBT). Patients learn to identify negative thoughts and feelings, and how to reframe and think more positively. You are encouraged to participate in activities that make you happy, especially during a depressive episode via (per NAMI). Many people with bipolar disorder avoid their triggers. CBT teaches them how to overcome avoidance, and learn to relax (via Psycom).
Another potential psychotherapy treatment is Interpersonal And Social Rhythm Therapy (IPSRT). As Stephen Ferrando, director of psychiatry at Westchester Medical Center Health Network (WMCHealth), told Psycom, IPSRT “helps individuals with bipolar disorder to understand what worsens and what triggers their illness.” ISPRT teaches patients how their actions affect their mood. For example, Dr. Ferrando mentions that the sleep disturbances caused by bipolar disorder often trigger episodes. So, patients may learn sleep management skills.
Family-focused treatment (FFT) enables loved ones to learn more about bipolar disorder, allowing for better relationships and helping those closest to the patient to figure out triggers and determine when medication isn’t taken as directed. FFT is best for those with depressive episodes (via MJA).
Medication treatment for bipolar disorder

taniascamera/Shutterstock
Lithium is one of the most common medications prescribed to treat both the mania and depression associated with bipolar disorder (via Psychiatric Times). It helps prevent symptoms and stabilize your mood. It also lowers your chances of dying from suicide, heart disease, cancer, stroke, vascular disease, and viral illnesses, all of which are seen at higher rates in those with bipolar disorder.
Another common bipolar medication is quetiapine. Sold under the brand name Seroquel, it is considered an antipsychotic and works better than lithium in patients with mixed manias and acute depressive episodes. It also helps with the anxiety and insomnia associated with bipolar disorder. Anti-depressants and anti-anxiety medications also get prescribed to those with bipolar disorder. However, because some anti-depressants trigger manic episodes, doctors may also prescribe a mood stabilizer or antipsychotic along with this class of drug. Medical providers prefer to prescribe anti-anxiety medicines for short-term use (via Mayo Clinic).
Because everyone is unique and responds to both bipolar disorder and the medicines to treat it in their own way, it takes time for your doctor to get your prescriptions just right (via Medical News Today). It often takes several tries with several different medications before the combination that works best for you is found. Additionally, it can take up to eight weeks for each drug to take full effect (via Healthline).
One important thing to keep in mind is that the drugs prescribed for bipolar disorder are associated with a higher risk of birth defects. Consult with your physician if you get pregnant or plan to breastfeed, or if you’re on birth control that might interact with your other medication.
Other medical treatments
Lana Leon/Shutterstock
If you fail to respond to medication and psychotherapy, your doctor may recommend you undergo electroconvulsive therapy (ECT). Performed in the hospital under medical supervision, this treatment is usually an outpatient procedure (via NYU Langone Health). Before beginning ECT, you are given a muscle relaxer and put under general anesthesia. Electrodes are then stuck to your head, and a low electric current causes you to go into a controlled seizure that lasts up to a minute.
The entire procedure lasts around 15 minutes. The seizures associated with ECT change the chemical makeup of your brain and reverse the symptoms associated with bipolar disorder (via Mayo Clinic). For best results, repeat the procedure monthly for up to a year (via Healthline). ECT is over 80% effective. It is also safe to use during pregnancy (via Healthline).
Another procedure that is being studied for use in patients is transcranial magnetic stimulation (TMS). Doctors use magnets to stimulate electrical activity in specific brain parts (via Medical News Today). TMS requires you to sit in a chair for up to an hour while a device sends magnetic pulses through your brain. It can take up to 25 sessions for TMS to be effective. As of this writing, TMS is moving through the FDA approval process.
Non-medical treatment

Rawpixel.com/Shutterstock
Medical professionals believe that up to 50% of those diagnosed with bipolar disorder or another mental illness self-treat using complementary and alternative medicine (CAM). Many incorporate these treatments with their prescriptions (via Psychiatric Times).
One way to help yourself live with bipolar disorder is to stick to a schedule (via Healthline). Your day should be structured, from when you wake up to when you go to sleep. Figure out the best times and foods to eat to boost your mood. You should try to stick to your routine and stay involved in activities, even when you don’t feel up to it. It’s also important to get moving. Though it is unclear why or how, studies show that exercise improves depressive symptoms, as well as your daily functioning and quality of life (via Journal of Affective Disorders).
While some herbs and supplements claim to alleviate symptoms associated with bipolar disorder, evidence of their safety and efficacy is hard to find (via Psychairctric Times).
If you or someone you know needs help with mental health or is having suicidal thoughts, please contact the Crisis Text Line by texting HOME to 741741, call the National Alliance on Mental Illness helpline at 1-800-950-NAMI (6264), visit the National Institute of Mental Health website, or call the National Suicide Prevention Lifeline by dialing 988 or by calling 1-800-273-TALK (8255).