Anorexia nervosa, also known as just anorexia, is a complex and serious eating disorder (via Current Opinion in Psychiatry). It’s reported all over the world and is estimated to affect up to 4% of women and 0.3% of men. The illness is primarily characterized by dietary restriction and an abnormally low body weight (via Nature Genetics). People with the condition become deeply preoccupied with what they eat and how much they weigh, often to the extent that it interferes with their day-to-day life. They may go to extreme lengths to lose and prevent putting on weight.
There are countless other symptoms that come along with anorexia, many of which can lead to death. It’s known to have one of the highest mortality rates of any psychiatric illness, but scientists are still uncovering its root causes. Read on to find out some of what we already know about this puzzling eating disorder.
If you are struggling with an eating disorder, or know someone who is, help is available. Visit the National Eating Disorders Association website or contact NEDA’s Live Helpline at 1-800-931-2237. You can also receive 24/7 Crisis Support via text (send NEDA to 741-741).
Signs and symptoms of anorexia

One of the main symptoms of anorexia is dietary restriction, often to the point of starvation (via Neuroscience & Biobehavioral Reviews). According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria, people with anorexia lose a lot of weight or fail to put it on (via National Library of Medicine). They have an intense fear of weight gain and a distorted perception of their body size and shape, which causes them to overestimate their weight. There are two sub-types of the illness: The restricting type and the binge-eating and purging type.
People with anorexia often engage in extreme and obsessive behaviors like counting calories, skipping meals, cutting out specific foods, or even using laxatives to control their weight. Other symptoms of anorexia include gastrointestinal problems, hair loss, muscle weakness, and low blood pressure and heart rate (via Journal of Eating Disorders). Some people may notice fine hair growing on different parts of the body like their back or the sides of their face. This is the body’s way of conserving heat when vital systems start to shut down as a result of malnourishment (via Cleveland Clinic).
It’s important to acknowledge that not everyone who’s suffering with the eating disorder will meet all of the diagnostic criteria, notes the National Eating Disorders Association. Like all mental conditions, the illness varies in its severity and clinical presentation from one individual to another.
What is atypical anorexia?

Eating disorder patients seldom neatly fit into a single diagnostic category. For this reason, a new category called “atypical anorexia” was created to account for those individuals who display most of the features of typical anorexia, except for an abnormally low body weight (via Journal of Eating Disorders). They may look relatively healthy rather than appearing emaciated — usually their weight will be within or above a normal range — which may lead others to believe they’re not “sick enough” to be considered anorexic. But like those with anorexia, they’ll be restricting their food intake, are similarly fixated on weight loss, and go to similar lengths to shed weight or avoid putting it on, yet they might think that they’re not “thin” enough. They’ll experience many of the same symptoms as people with anorexia like gastrointestinal problems, a low immune system, fatigue, and low mood.
Around 40% of people with atypical anorexia end up being hospitalized, and they make up nearly one-third of eating disorder inpatient admissions (via Pediatrics). These individuals can easily go under the radar because they’re not underweight, and it’s generally assumed that their eating disorder is less serious than those with anorexia (via Journal of Eating Disorders). But the truth is, the psychological distress that people with atypical anorexia experience can be just as bad, if not worse, and the medical consequences are often just as damaging and deadly. Those with atypical anorexia are also less likely to receive inpatient care and tend to have a longer duration of illness.
Who is at risk for anorexia nervosa?

chaipong pramjit/Shutterstock
Anorexia was once perceived as a Western middle class problem (via Topoi). But while it’s more frequently reported in high-income Western countries, it’s clear that the disorder can affect people of all nationalities and socioeconomic backgrounds.
According to statistics, anorexia typically begins in adolescence and mostly affects women, per the National Eating Disorders Collaboration. This is reinforced by the fact that there’s generally more societal pressure to look a certain way placed on women than on men (via Medical News Today). However, the stigma surrounding eating disorders, particularly among male survivors, might mean that a lot of people suffer in silence, making it difficult to gauge true prevalence rates.
Certain environments may raise the risk of developing anorexia (via the National Eating Disorders Collaboration). For instance, the eating disorder tends to be more common among people working in industries where there’s profound pressure to be of a certain weight and appearance in order to be successful, like athletes and models. People with first-degree family members with anorexia are also said to have a 10-fold greater risk of developing the disorder themselves (via Cleveland Clinic Journal of Medicine).
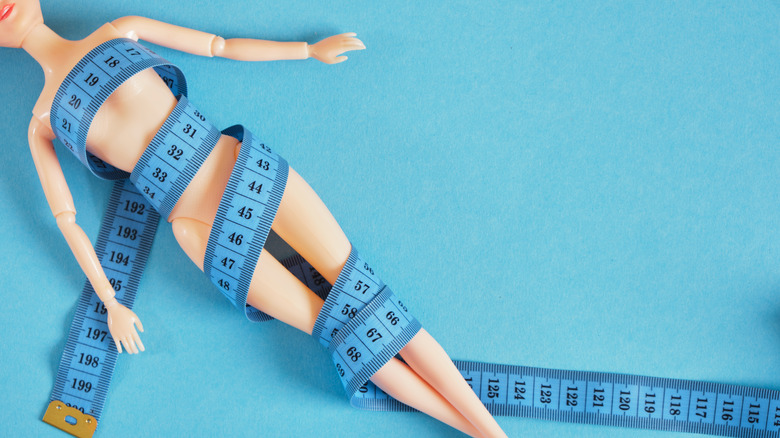
Social factors that may contribute to anorexia

tommaso79/Shutterstock
Scientists have been investigating the underlying causes of anorexia for decades (via Science). It’s generally agreed that the disorder is multifactorial — in other words, it probably stems from a complex interaction of factors rather than just one cause, and these may differ across individuals (via Topoi). But there’s strong evidence that sociocultural influences can play a pretty big role. For instance, anorexia tends to be more common in Western or westernized societies, where people face greater cultural pressures to be thin and there’s a stronger emphasis on achieving the “perfect body.”
Time and time again, thin-ideal internalization has been shown to predict the onset of anorexia (via Journal of Eating Disorders). Very specific standards of beauty and physical attractiveness are often prominent in media, and it’s natural and common for individuals to buy into these societal ideals over time. This can lead to excessive dieting and exercising, lower body satisfaction and bodily awareness, and an increase in disordered thinking and eating behaviors.
Genetic factors underlying anorexia

Akkalak Aiempradit/Shutterstock
Genetics may very well play a role in the development of eating disorders. Findings from twin studies estimate that the heritability of anorexia is somewhere between 50% and 60% (via Nature Genetics). Researchers have identified eight chromosome locations that may point to an increased vulnerability to the illness, and it’s suggested that there are probably many more. Some of these genetic loci have been linked to metabolic problems, while others are associated with psychiatric disorders.
But while a person’s genes might make them much more susceptible to developing anorexia, this is only one piece of the puzzle, say researchers (via Biological Psychiatry Global Open Science). It’s likely that eating disorders arise from a number of different factors, including genetic, psychological, and environmental. Still, getting a better understanding of the genetic origins of anorexia could be a valuable step toward designing novel treatments, researchers point out. The disorder is known for being notoriously hard to treat (via Topoi).
The role of the family

Prostock-studio/Shutterstock
Anorexia has been found to be more prevalent within dysfunctional family environments (via Topoi). People with anorexia often report growing up around a lot of family conflict and stress, where there’s a great deal of disagreement among family members. The families of anorexics tend to value competitive success in areas such as school and professional life. Yet, they might also encourage their children to be submissive and conforming, often at the expense of their own boundaries.
Parents that show intrusive or withdrawing behaviors in the first five years of their child’s life may contribute to the development of an eating disorder during adolescence, according to a review study published in Behavioral Sciences (Basel). This is especially true for parents who have a personal history of trauma and physical and/or psychological abuse in childhood.
Research also highlights a strong connection between trauma and anorexia: Survivors of childhood abuse are more prone to bodily disturbances and poor body image, which are major predictors of anorexia (via Health Care for Women International). From a family-based perspective, anorexia can develop as a sort of coping mechanism in problematic families and as a “defense mechanism” in highly stressful environments (via Topoi).
Psychological risk factors
Evgeny Atamanenko/Shutterstock
As with most mental health conditions, there’s a large psychological component to developing anorexia, claim researchers (via Cognitive, Affective, & Behavioral Neuroscience). People who go on to develop the illness are usually quite perfectionistic and black-and-white in their thinking. They have low levels of self-esteem and a poor sense of control.
Perfectionism can lead people to be more critical and less forgiving of themselves. They make harsher-self-evaluations. So, they might perceive themselves as being overweight when in fact their weight is already dangerously low. Restricting what they eat can be a way for them to feel more in control and confident in their lives. People with high levels of perfectionism and low self-esteem also give more importance to appearance than others (via Journal of Eating Disorders). They base their self-worth on their ability to achieve things perfectly, including the “ideal body.” Perfectionistic people are more likely to internalize the “thin ideal” and surround themselves with peers who also value and pursue thinness, both of which are risk factors for anorexia (via International Journal of Eating Disorders).
The neurobiology of anorexia

Pixel-Shot/Shutterstock
Researchers have discovered that people with anorexia have structural and functional differences in certain regions of the brain, such as the orbitofrontal cortex (via The Journal of Neuroscience). This area is involved in decision-making, specifically about what to eat, as well as evaluations of the tastiness and healthiness of different foods.
Individuals with anorexia also appear to engage the dorsal striatum more than healthy controls do when thinking about what to eat, reports a 2024 study (via The Journal of Clinical Investigation). This part of the brain is associated with habitual actions. Using a computer-based neurocognitive task, the researchers showed that people with restrictive anorexia are more prone to habitual and maladaptive behaviors than healthy individuals.
Another region of the brain that functions differently in anorexics is the right insula (via Neuropsychopharmacology). This area regulates both taste sensations and interoception, which is the ability to connect to one’s internal signals. People with anorexia may have visceral hypersensitivity. This means they notice their body’s sensations and physiological signals much more than others, resulting in heightened anxiety. Food restriction and starvation may be coping responses to this — a way to quieten internal bodily noise.
Anorexia and malnutrition

Long-term anorexia can lead to malnourishment (via Internal and Emergency Medicine). The body can become extremely frail and unwell due to a lack of nutrients caused by food restriction. Some patients get so malnourished that they need to be hospitalized.
In the beginning stages of an eating disorder, a person might restrict what they eat to reach a certain weight. But anorexia can trick the individual into thinking that they haven’t lost enough weight and need to keep starving themselves (via Topoi). They might believe that they don’t need the same amount of nutrients as others, or they may dismiss the consequences of being undernourished. Some of the side effects of malnourishment include dry skin, shortness of breath, poor concentration, feeling cold all the time, delayed wound healing, bradycardia, and hypotension (via Journal of Eating Disorders). In the long term, the complications can be a lot more severe, affecting the cardiac, hematologic, and musculoskeletal systems (via Internal and Emergency Medicine).
In order to restore the body’s depleted nutrients, hospitalized patients are re-fed (via Internal and Emergency Medicine). However, the process of reintroducing food too quickly can be dangerous, and in some cases, deadly. A sudden change in metabolism can trigger various hormones and cause a shift in electrolytes and other chemicals. This is known as “refeeding syndrome.” After being in starvation mode for so long, the body needs time to readjust. Around 33% of patients with anorexia experience refeeding syndrome, and in some cases this is fatal.
Dangers and complications of anorexia nervosa

CGN089/Shutterstock
Anorexia is one of the deadliest psychiatric conditions out there, according to research (via Cleveland Clinic Journal of Medicine). Around 5% of anorexia cases result in death, and 20% of those deaths are due to suicide. People with the illness put their bodies under a huge amount of physical and psychological stress. They often engage in dangerous and potentially life-threatening behaviors such as starving themselves or severely restricting the amount of food that they eat. Some people also binge, purge, and excessively exercise. All of this has an inevitable knock-on effect on health.
Some of the dangers of anorexia include heart failure, muscle wastage, and loss of bone density due to poor nutrition (via Cleveland Clinic Journal of Medicine). Most complications can be reversed throughout recovery as people gain weight and receive nutritional therapy. However, struggling with the illness for a long period of time can lead to permanent health issues even after treatment and recovery, like the brittle bone disease osteoporosis.
Some patients have been known to experience brain atrophy and damaged gray and white matter, which can result in long-term cognitive impairments. Anorexia can also lead to infertility. Female anorexia patients often stop menstruating and have low estrogen levels, while male patients have low testosterone.
If you or anyone you know is having suicidal thoughts, please call the National Suicide Prevention Lifeline at 1-800-273-TALK (8255).
Anorexia and the menstrual cycle
TShaKopy/Shutterstock
Amenorrhea — the absence of menstruation in a woman of childbearing age — is a common side effect of anorexia (via Journal of Clinical Medicine). It occurs in up to 84% of women with the eating disorder. When the body goes into survival mode and starts experiencing various hormonal changes, a woman stops having her period — meaning she’s also temporarily unable to have babies. Another pretty serious consequence of this is a drop in estrogen levels. This can affect a woman’s mood, weight, and ability to sleep. A lack of estrogen production can also cause a massive depletion of calcium in the bones known as osteopenia, the precursor of osteoporosis.
Secondary amenorrhea is when a woman has stopped getting her period for at least three or more months in a row (via Kantor & Kantor). This used to be part of the diagnostic criterion for anorexia nervosa but was dropped in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM) for a number of reasons. Firstly, not all women with the illness will stop having their period. This criterion also excluded men as well as women who are very young, post-menopausal, or using hormonal contraceptives.
What psychological conditions occur alongside anorexia?

Anorexia can massively harm an individual’s body and mental health. It’s no surprise, then, that the condition often comes along with other medical and psychological issues. Around 56-95% of people with an eating disorder end up getting diagnosed with at least one other psychiatric illness, according to the National Eating Disorders Collaboration.
The most common psychiatric comorbidities associated with anorexia are mood disorders like depression and anxiety (via Frontiers in Psychiatry). Around 72% of anorexia patients have generalized anxiety disorder (GAD), 64% struggle with major depressive disorder (MDD), and up to 62% have obsessive-compulsive disorder (OCD). Mood disorders are more commonly seen in people who have the binge/purge subtype of anorexia than in the restrictive subtype, per Harvard T.H. Chan.
Anorexia symptoms are usually more severe in patients with a comorbid disorder of MDD, GAD, or social phobia (via Frontiers in Psychiatry). There’s evidence that added emotional difficulties associated with anxiety and depression make it harder for people to make good decisions, which can also affect decision-making around food choices.
Treatments for anorexia

Photographee.eu/Shutterstock
Even though anorexia can have life-threatening consequences, it’s important to acknowledge that recovery is entirely possible, particularly when it’s treated early (via Frontiers in Psychiatry). Up to 50% of people who receive treatment in adolescence recover from the illness. Treatment is usually made up of both talking therapy and supervised weight gain (via Clinical Therapeutics). However, the idea of gaining weight can trigger a lot of anxiety in patients, creating a barrier to the recovery process.
Family-based treatment (FBT), also known as the Maudsley method, is the go-to outpatient intervention for anorexia, particularly for adolescents. It conceptualizes the family as playing a key role in both the etiology and treatment of the disorder. Parents and other family members are typically involved in the therapy sessions.
Cognitive behavioral therapy (CBT) is another effective, evidence-based intervention that helps tackle the disordered cognitions, beliefs, and behaviors behind anorexia. Patients learn how to cope with their emotions, gain a better understanding of nutrition, and develop healthier eating habits. The goal of therapy is to help individuals understand what drives their illness and to feel more comfortable with food and their body so that they can reach a healthy weight.
If you think you might have anorexia, get in touch with your doctor to discuss the type of therapy that’s available to you. There’s no single best way to treat eating disorders — different treatments will work for different people.
If you are struggling with an eating disorder, or know someone who is, help is available. Visit the National Eating Disorders Association website or contact NEDA’s Live Helpline at 1-800-931-2237. You can also receive 24/7 Crisis Support via text (send NEDA to 741-741).