Sleep is a mysterious thing. Honestly, shutting your eyes and waking up eight hours later, with all of that time just gone? Pretty wild. But what happens when we sleep affects the quality of our lives significantly, and certain sleep conditions can be incredibly impactful, whether we know we have them or not. Sleep apnea is one of these conditions.
Affecting between 10% and 30% of all American adults (per research published via UpToDate), sleep apnea is characterized by temporary lapses in breathing during your sleeping hours, either down to an obstruction to your airways or because of disrupted brain signals, as the Sleep Foundation explains. These breathing pauses can have a knock-on effect on the quality of your sleep, creating difficulty concentrating or focusing the next day, making you feel more tired, and giving you morning headaches.
The strangest part is, many people don’t even know they have sleep apnea in the first place, due to their breathing pauses not being severe enough to wake them up entirely. So with a condition as elusive as this, it’s perhaps natural that myths have spread about it. That’s why we decided to put to bed, once and for all, the mistruths and rumors around sleep apnea, and give you the facts.
Myth: You can’t have sleep apnea if you don’t snore

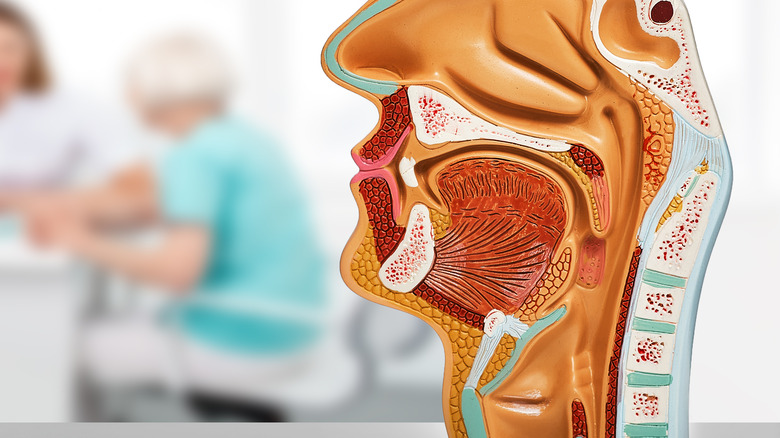
When most people think of sleep apnea, they associate it with a large amount of snoring, one of the condition’s key symptoms (per the Mayo Clinic). Snoring occurs thanks to one of the causes of obstructive sleep apnea: The throat muscles collapse, creating an abundance of soft tissue that makes your airways smaller, according to Chidinma Chima-Melton, University of California Assistant Professor of Clinical Medicine in the Pulmonary and Critical Care Division (via WebMD).
Because of this, it must be logical to think that if you’re not snoring through the night, then your airways aren’t collapsing, and therefore you’re not experiencing sleep apnea. Right? Wrong. It’s entirely possible to have sleep apnea without snoring, especially if you have central sleep apnea, a variation on the condition that results in lapses in breathing not because of a closed throat, but because your brain fails to transmit to your breathing muscles that they need to operate consistently in sleep.
Instead, it’s wise to look out for other telltale signs of sleep apnea, like fatigue and headaches during the day and waking up gasping at night. Seeking treatment if you have these symptoms can provide significant improvements to your quality of life.
Myth: You should just live with your apnea

When it comes to sleep apnea, it can be tempting to write it off as a mere inconvenience. After all, who hasn’t woken up a few times in the night and felt a bit tired the next day? It’s important to remember, though, that the consequences of sleep apnea extend far beyond being a little groggy.
Experiencing sleep apnea consistently can lead to a range of more profound health concerns, such as elevated blood pressure and higher risk of cardiovascular disease, as well as increased likelihood of stroke, says the NHS. Your mental health can be impacted too, with a heightened risk of developing depression. Moreover, your sleep apnea may not be affecting just you. Your consistent tiredness and fatigue can also put a strain on relationships with those around you — not least with the person you might share a bed with — especially if they’re kept awake by apnea symptoms like snoring.
Finally, bear in mind that apnea puts you at greater risk of making errors in judgment during the day, potentially impacting your work and impairing decisions you make (like while you’re driving or operating heavy machinery).
Myth: Sleep apnea always blocks your airways

Pixel-Shot/Shutterstock
Think sleep apnea, and you’ll likely think of obstructive sleep apnea; far and away the most common form of the condition, this happens when your breathing is stopped by your throat closing in the night (per the Mayo Clinic). But that’s not the only type you need to know about.
Central sleep apnea, which is rarer, is due to the connection between your brain and sleeping muscles not functioning correctly (per Sleep Foundation). As a result, your muscles temporarily pause in their efforts to keep the breath moving in and out of your body, and you stop breathing.
Central sleep apnea is more frequent in older patients and men, and can commonly occur in tandem with an underlying condition like stroke or cardiovascular disease, according to research published in UpToDate. It may also happen thanks to certain drugs or substances, particularly opioids, which tend to suppress the part of the brain that regulates the sleep muscles.
Like obstructive sleep apnea, central sleep apnea can have a serious impact on your waking hours, and it’s important to address it if you notice any of its symptoms.
Myth: Sleep apnea only affects adults

Chinnapong/Shutterstock
For one reason or another, sleep apnea can be considered an adult-only condition, and a common myth around it is that kids can’t have it. And while that may be a comforting thought to parents worldwide, unfortunately, it isn’t the case.
Pediatric obstructive sleep apnea is a form of the condition that affects children, which happens due to the airways becoming blocked, as is the case in adult obstructive apnea (per the Mayo Clinic). In kids, this obstruction is generally due to the tonsils or adenoids being larger, and surgery on one or both of these areas may be recommended to treat the apnea (per UpToDate).
Bear in mind that unlike adult apnea, kids generally don’t exhibit daytime sleepiness as one of its main symptoms. Instead, it’s more common to show signs that could be mistaken for a behavioral condition, like a lower capacity for paying attention to school subjects or having poorer grades. They may also seem more awake during the day, with hyperactivity a telltale sign of obstructive sleep apnea in children. You must consult with your pediatrician if you suspect your child has sleep apnea, as long-term complications from the condition can be profound, ranging from growth difficulties to cardiovascular issues and even death.
Myth: Sleep apnea is only affected by your weight

Prostock Studio/Shutterstock
How much you weigh can have an enormous impact on whether you develop sleep apnea or not, with obesity being “the biggest risk factor for sleep apnea,” sleep expert Susheel P. Patil states (via Johns Hopkins Medicine). But that’s not to say it’s the only thing that impacts your likelihood of having the condition, and you could still have obstructive sleep apnea even if not overweight. The composition of your facial features may make the condition more likely, and folks with a smaller chin or jaw that’s set further back into the face might be more prone to apnea. This may also be the case if you have a significant overbite.
Your neck plays a big part too, and people with larger necks can frequently have smaller airways, meaning more likelihood of obstruction (per ResMed). Generally, men with a neck width of 17 inches or over, and women whose neck circumference is 16 inches or above, are at higher risk of apnea. Particularly large tonsils may also be a risk factor, as they can interfere with your airways, according to Mount Sinai.
Myth: If you had the condition, you’d know about it

Fizkes/Shutterstock
It’s not an over-exaggeration to say that sleep apnea is a pretty dramatic condition, what with the stopping-breathing-in-the-night aspect and all that. And as such, you’d be forgiven for assuming that if you cease your breathing in the night, you’re going to notice it, fast.
But the thing is, most people don’t notice it. “Sleep apnea is grossly under-recognized. We estimate that 85 to 90 percent of people with sleep apnea in this country don’t know they have it,” states the director of the Cleveland Clinic Sleep Disorders Center Nancy Foldvary Schaefer (via Cleveland Clinic). This is largely because the symptoms of sleep apnea, when mild, are pretty subtle, with tiredness during the day or a headache in the morning being common. These symptoms are often missed by both patients and doctors, and given that sleep medicine is a specialized zone of medicine and your doctor may be pushed for time, it’s all too easy for apnea to be missed.
Given that untreated sleep apnea can have a progressive impact on other parts of your health, however, it’s vital that if you suspect you have it, you tell your doctor at the first opportunity.
Myth: Mild sleep apnea is less impactful

Prostock Studio/Shutterstock
It’s easy to assume that if your sleep apnea is defined as mild, it’s barely worth mentioning or indeed addressing. But that couldn’t be further from the truth.
Sleep apnea is classified into three different categories — mild, moderate, or severe — based on where you place on something called the “apnea-hypopnea index” (say it out loud, it’s pretty fun, honestly) or AHI, according to Harvard Health Publishing. Where you fall on the AHI tells you, essentially, how many times you experience disrupted sleep or wake up every hour.
The majority of people place in the mild category on the AHI index, but the problem is that doesn’t mean your symptoms are mild, too. People can still be classified as having “mild” sleep apnea and have signs that they might assume place them in a moderate or severe category, with extensive difficulties with sleep and real trouble staying awake during the day. Conversely, a person can be diagnosed as having “severe” sleep apnea and barely notice any impact on their quality of life. It’s worth noting that your doctor may not get your treatment plan right the first time, and if you have mild sleep apnea and what you’ve discussed with your doctor isn’t working, there’s no shame in going back and asking for a reassessment of how you manage your condition.
Myth: If you snore, you have sleep apnea

Tommaso79/Shutterstock
Turning to your partner and asking them the big questions in life can strengthen a relationship, but sometimes, you may not like what you hear. And if you’ve ever plucked up the bravery to ask “Do I snore?” and been faced with a solemn nod, you’ll know it’s a moment of serious reflection.
This process of reflection might prompt you to examine why you’re snoring in the first place, and as snoring is commonly associated with obstructive sleep apnea (per the Mayo Clinic), it’s easy to assume that’s the cause. Remember, though, that’s not the only reason you’re a loud sleeper. Your likelihood of snoring can be affected by anything from the position you sleep to your body composition. If you’re frequently congested or have a deviated nasal septum, you could be more likely to breathe roughly. The shape of your mouth can play a big part too, with thicker soft palates producing increased difficulty breathing in sleep, causing snoring.
You may also snore more if you drink alcohol before going to bed, as this may prompt your airways to become narrower. The same thing can happen if you sleep less than you should. If you’re concerned about your snoring, it’s important to discuss it with a doctor, instead of self-diagnosing with sleep apnea.
Myth: Your apnea only happens in certain sleeping positions

Ground Picture/Shutterstock
If you have sleep apnea, you may be familiar with the feeling of a well-intentioned but frustrated partner’s hand descending on you in the night, urging you to turn over in bed, to stop you from snoring. But the fact of the matter is that sleep apnea can occur no matter what side of your body you sleep on, according to Silent Night Therapy.
With that said, there are adjustments you can make to your sleeping position that could improve your sleep apnea symptoms. “Sleep apnea is often worse in the supine (on your back) position because of gravity,” states National Jewish Health section head of sleep medicine Sheila Tsai (via U.S. News). This is because when you’re on your back, it’s easier for your tongue to obstruct your airways. Sleeping on your side or your stomach, however, may alleviate symptoms, and in some cases could reduce them significantly.
Your neck and head position are also important, and positioning them in a more elevated position may assist in keeping your apnea manageable, especially if you’re prone to sleeping on your back.
Myth: Sleeping medication can help sleep apnea

Svetlichniy Igor/Shutterstock
People with sleep apnea will know how hard it can be to sleep soundly sometimes. And logically, they may start to think about ways they can get a good night’s rest. That’s why it’s easy to conclude that sleeping medication could be the miracle cure they’re looking for — but we’d advise against using sleeping pills to manage your condition.
The problem lies in the origins of sleep apnea itself: It is often caused by a relaxation of your mouth and throat muscles, leading to a blockage of the airways and a pause in breathing (per Weatherford Dental Sleep Medicine). But sleeping pills also act to relax the body and mind, and this then means that you’re making your facial and throat muscles slacken even more. Therefore, while you might assume that sleeping meds will make you feel refreshed, they may make your symptoms worse. This could even lead to some of the more profound negative side effects of sleep apnea, like noticeable exhaustion, poor mood, cardiovascular complications, and a higher chance of developing diabetes. Discussing your options with a sleep expert instead of reaching for sleeping medication is highly advised.
Myth: Sleep apnea only affects men

Andrey Popov/Shutterstock
Somewhere along the line, the perception of sleep apnea as a male condition gained traction (per Johns Hopkins Medicine). But this isn’t strictly true. It is certainly the case that sleep apnea is far more common in men than in women, with between double and triple the amount of cases of apnea in men, according to the Mayo Clinic. However, this may well be because women tend to be less likely to report symptoms of sleep apnea in the first place, leading to underdiagnosis overall, says sleep expert Susheel P. Patil.
Snoring, one of the main symptoms of sleep apnea, may be harder to notice in women than in men, and also may not be reported by women as often as men do. The other signs of sleep apnea may also be conflated with other conditions, and this may mean that women are diagnosed differently. Women’s likelihood of developing sleep apnea can change as their lives develop, and post-menopausal women are more prone to the condition, Patil states.
Myth: CPAP machines are the only treatment

Kateryna Mostova/Shutterstock
Sleep apnea is frequently treated with the use of a CPAP machine, and they can provide enormous relief for individuals who experience apnea issues (per Healthline). CPAP (continuous positive airway pressure) machines operate via a mask attached to your face while you sleep, which pumps a constant supply of air into your airways, thereby keeping them open.
Because to their efficacy in treating sleep apnea, though, it’s often assumed that’s the sole way that symptoms can be relieved — and in fact, there are a host of treatments out there. Adjustments to weight or surgical procedures that get rid of tissue that causes the air blockage are two viable forms of treatment that may relieve sleep apnea without the need for wearing a mask, says Shore Medical Center. Dental inserts may also be recommended by your doctor, which serve the same purpose.
And even if you do opt for help from a CPAP machine, it’s a misconception that all CPAP masks are enormous and unwieldy. CPAP appliances come in all shapes and sizes, and may cover your nose or be inserted into your nostrils, depending on what works best for you.
Myth: Alcohol can help ease your symptoms

Kmpzzz/Shutterstock
A nightcap after a long day is a time-honored tradition for millions of people, and serves as a way to relax before you go to sleep. And for people with sleep apnea, it’s often assumed that alcohol, with its seeming ability to set a person up for a good night’s rest, may allow them to sleep through the night. But self-prescribing alcohol for sleep is not only risky business, but will also do nothing to help your apnea — and is likely to make it worse.
Research published in Sleep Medicine indicates that drinking alcohol creates a higher likelihood of sleep apnea, potentially because alcohol acts as a muscle relaxant and reduces the speed at which you wake up. This means that apnea episodes are longer and more frequent (per Sleep Care Online). There’s also the fact that, contrary to popular belief, alcohol doesn’t give you that restful night’s sleep that you require. Drinking booze works to lower your levels of melatonin — the hormone that’s so crucial to a good slumber — and while you may drop off quicker, your sleep is likely to be more unsettled.
Myth: You won’t get sleep apnea if you don’t have tonsils
Peakstock/Shutterstock
Your tonsils are tricky things, and for one reason or another, many people opt to have them removed via tonsillectomy. And given that taking our your tonsils means you have more space in your mouth and throat, it’s commonly assumed that this means that you’re no longer at risk of obstructive sleep apnea. Unfortunately, folks, this isn’t the case, as whether you have tonsils or not, you can still get the condition (per Silent Night Therapy).
It’s certainly true that tonsillectomies can treat sleep apnea if your tonsils are the cause, as Healthline states, but they’re only responsible for the condition in certain cases. Sleep apnea can be prompted by excess tissue in the throat and mouth, which a variety of other surgical procedures can address, like a (deep breath here, people) uvulopalatopharyngoplasty, which address the areas around your uvula and soft palette, and a septoplasty, a type of surgery that aligns your nasal septum. If your sleep apnea is a result of your jaw alignment, surgeons may perform a jaw repositioning, shifting it forward slightly so your throat opening has more space.



